
CMO Corner: Lawrence Magras, MD, MBA, FHM, FAAPL
Recent data from the Centers for Disease Control and Prevention (CDC) ranks Chronic Obstructive Pulmonary Disease (COPD) as the third leading cause of death, affecting 15.7 million Americans. According to Connecticut Behavioral Risk Factor Surveillance System (CT BRFSS), a survey utilized by the CDC to collect state data on chronic diseases, over 6% of Connecticut State adults reported that they had been informed they had COPD. HUSKY Health data on hospital admissions and readmissions over the past three years demonstrates that COPD continues to be a significant driver of hospital encounters with a sustained readmission rate of 20%. Additionally, due to high emergency room and hospital utilization, research shows that about 10% of COPD patients account for 70% of costs in this patient population. . . read more
In response, CHNCT’s Quality Management team has identified several areas for improvement for this preventable chronic disease. Through effective disease prevention activities and timely management of COPD, affected members can experience a reduction in disease progression, complications, and disease comorbidities.
By using a focused approach, through a quality improvement project, our goal is to reduce hospital encounters, improve member quality of life, and decrease chronic care costs. Specific actions include development and implementation of a series of interdepartmental process improvements focusing on more effective prevention strategies, safer transitions of care, and enhanced post-hospitalization follow-up. Interventions will include implementation of improved COPD care pathways, COPD action plans, spirometry testing, as well as the development of disease-specific patient education and self-management materials, including vaccine promotion.
Community Health Network of Connecticut, Inc. (CHNCT) will reinforce COPD best practices with providers, and highlight specific factors and processes that promote respiratory wellness with members. CHNCT’s Intensive Care Management (ICM) staff will utilize the recently updated HUSKY Health website to disseminate provider education materials and to encourage provider referrals to spirometry testing and pulmonary rehabilitation. Through increased awareness of COPD assessment techniques and optimal strategies to manage COPD, providers will provide better care to HUSKY Health members and may ultimately reduce exacerbations rates.
Watch for Fall 2017 Continuing Medical Education (CME) Opportunities!

Cultural Competence at Your Fingertips
Today’s healthcare professionals see more and more patients from diverse cultural backgrounds. Understanding their particular needs is critical to providing complete care. The more you know a person’s healthcare beliefs or practices, the more your care and treatment plans can be designed for the best health outcomes possible. With this information, you can take your patients’ worldview into account. . . read more
CultureVision™ is an easy to use database that gives healthcare professionals access to culturally competent patient care. Nothing to install. Nothing to download.
HUSKY Health offers free access to CultureVision through our Secure Provider Portal. To access the portal, click here. To sign up for an account, follow the instructions in this how-to-guide.
Once you log in, click the CultureVision link. You can begin using the service immediately.
CultureVision can help you:
- Improve Quality of Care: Access information about the prevalence of diseases within certain populations and provide guidance in understanding cultural influences on what patients believe will make them well.
- Reduce Disparities: Identify impact of cultural issues on medical decision-making and limit inadvertent bias in diagnosis and treatment.
- Increase Patient Satisfaction: Identify questions to ask that will elicit pertinent information and improve communication where language barriers may exist. Effective and efficient communication between a provider and patient will inform treatment planning and ultimately improve patients’ health outcomes.
Source: http://www.crculturevision.com
Attention PCPs: Adult Diabetes Screening Tests – Gaps in Care Available on the HUSKY Health Secure Provider Portal
As a Primary Care Provider (PCP), we want you to have direct access to data on your attributed HUSKY Health members. The HUSKY Health secure provider web portal provides you with a variety of reports on your attributed members regarding their gaps in care, cancer screenings, ED utilization, and much more. . . read more
One key report is the “Adult Diabetes Screening Tests - Gaps in Care” report, which identifies your attributed members ages 18 to 75 years of age who have a diagnosis of diabetes or prescription for any diabetic medication reported within the last two years, and would be considered to have Type 1 or Type 2 diabetes. The report shows you the last service date for HbA1c and Nephropathy testing, or a retinal eye exam with an eye care professional. This report enables you to schedule the member for services or to engage them in follow-up care in a timely fashion. You can also see if your member is currently enrolled in the HUSKY Health Intensive Care Management (ICM) program.
ICM provides comprehensive care coordination services for members with multi-morbid chronic conditions. Our nurses work directly with you and your HUSKY Health patients to manage their conditions using a person-centered approach. To learn more about ICM, click here. To refer HUSKY Health patients to ICM for additional support, use our ICM Referral form. To follow-up on patients who are enrolled with ICM, please contact us at 1.800.440.5071 x2024.
To access the reports, you must first set up an account on the HUSKY Health portal by visiting portal.ct.gov/husky, clicking “For Providers,” then “Provider Login.” Once you have an account, you will be able to request access to your reports. You will be notified via email when your report(s) are available for viewing. To learn more about how to gain access to the Provider Portal Reports, click here.

HEDIS® Update
Community Health Network of Connecticut, Inc. (CHNCT), contracts with the State of Connecticut Department of Social Services (DSS) as the Medical Administrative Services Organization for the HUSKY Health program. Annually, we request medical records from specific providers to monitor the quality of care and services as defined by Healthcare Effectiveness Data and Information Set (HEDIS®). As of May 2017, we have received the requested medical records and abstracted the necessary data. This information will be shared with the National Committee for Quality Assurance (NCQA), as well as DSS. . . read more
CHNCT would like to thank all of our providers and associated staff who participated in the annual HEDIS® data collection. Thank you for your assistance with the medical record requests and follow-up phone calls, emails, and onsite visits. We certainly understand that these requests can be overwhelming at times and we appreciate your patience and understanding.
As you know, healthcare consumers are relying on measurable data that illustrates the quality of care and services. Consumers are looking for care that is accessible, provides the consumer with informed choices, and encourages accountability. By providing us with your information, we are able to assess and develop action plans to improve the care for our members.
Thank you again for your cooperation and efforts during the HEDIS® data collection process.

Using Periodic Counseling to Help Patients Quit Smoking
Department of Social Services (DSS) Person-Centered Medical Home program participant practices are required to address smoking cessation with their HUSKY Health patients
To achieve this, HUSKY Health recommends smoking cessation counseling. Multiple treatments for tobacco cessation are more effective than using one alone1. The average smoker who successfully quits smoking is usually unsuccessful in 5 previous attempts, so it is important to keep trying. . . read more
To support you with smoking cessation counseling efforts, DSS is reimbursing two CPT codes for smoking cessation counseling for members enrolled under HUSKY A, C, and D. However, smoking cessation counseling will only be covered for HUSKY B members who are pregnant. Smoking cessation is reimbursable when provided by an enrolled physician, physician assistant,2 APRN,2 behavioral health clinician, medical clinic, mental health clinic, or family planning clinic. These codes are eligible for reimbursement supplemental to many other services commonly rendered during an office visit on the same day. Any evaluation and management services reported on the same day must be distinct and reported with modifier 25. A Federally Qualified Health Center (FQHC) must bill the encounter code T1015 with the modifier 25.
Billing codes to use for smoking cessation counseling reimbursement:
| CPT Code3 | Description |
|---|---|
| 99406 | Smoking and tobacco cessation counseling visit; intermediate, greater than 3 minutes up to 10 minutes |
| 99407 | Smoking and tobacco cessation counseling visit; intensive, greater than 10 minutes |
| 994124 | Preventive medicine counseling and/or risk factor reduction intervention(s) provided to individuals in a group setting; approximately 60 minutes |
Smoking Cessation Assistance Supported and Covered by HUSKY Health:
- Individual face-to-face or group smoking cessation counseling
- Nicotine replacement products (inhalers, lozenges, nasal sprays, and patches)
- Prescription Medications:
- Bupropion SR (Wellbutrin XL)
- Varenicline (Chantix)
To assist you with your smoking cessation efforts with your HUSKY Health patients, we also encourage you to promote the CT Quitline 1.800.QUIT.NOW (1.800.784.8669). Visit our website (portal.ct.gov/husky) for additional resources, including a free quit smoking app that patients can download to their mobile devices.
Additional Information
Visit: portal.ct.gov/husky and click “For Providers,” then “Smoking Cessation” under the “Person-Centered Medical Home” menu item.
1 Fiore MC, Jaén CR, Baker TB, et al Treating Tobacco Use and Dependence: 2008 Update—Clinical Practice Guidelines. Rockville (MD))
2 If an APRN or PA is performing the service, they will be reimbursed at 90% of the physician fee.
3 Claim must include an ICD-10 tobacco-related primary diagnosis code (Primary) Nicotine Dependence series: F17.20-F17.299 (Secondary) Smoking (tobacco) complicating pregnancy series: O99.330-O99.333
4 FQHCs should use encounter code T1015 when billing for smoking cessation group counseling. For FQHCs, the minimum number of individuals to comprise a group is three. The maximum number of individuals in any smoking cessation group, regardless of payer, is 8 individuals, not including the professional facilitating the group. This code can only be used when the duration of the group meets or exceeds 45 minutes and the individual has attended the session for the entire 45 minutes.

Intensive Care Management Support for Members At-Risk for Postpartum Depression
The Healthy Beginnings Intensive Care Management (ICM) program is available to help support your patients through the prenatal and postpartum period. Our nurses have clinical training in perinatal care with a focus on educating members on the benefits of self-care, as well as empowering members to improve their health and wellness. . . read more
When members enter the voluntary program, ICM completes a holistic assessment with the member to help better understand their needs. ICM has a tool within the assessment to help identify members who are at risk for postpartum blues, postpartum depression, and postpartum psychosis. The use of My 9 Months magazine, an evidence-based teaching tool from the March of Dimes, is sent to members as a supplement to the coaching the member receives on postpartum depression.
The Healthy Beginnings program offers multiple ways to build rapport with our members and assess their needs. The program offers interaction both in-person and through telecommunication. During these contacts, members receive coaching on self-care topics including recognizing and accessing help with postpartum depression.
The ICM program has an assessment tool designed to ascertain information similar to that of the Edinburg Postnatal Depression Scale (EPDS) which was mentioned in the Connecticut Department of Social Services (DSS) Provider Bulletin PB 2016-63 - October 2016. We also conduct a depression screen to determine whether the member has had signs and symptoms of depression.
When we identify a behavioral health concern, our Intensive Care Manager can provide a warm transfer call to the Connecticut Behavioral Health Partnership (CT BHP).
We discuss complicated cases in monthly meetings comprised of a multidisciplinary team to lend support to care managers, which ultimately provides the care managers with a dynamic pool of knowledge to assist members.
Collaboration with providers is important for the member to receive comprehensive, coordinated care. The ICM program supports providers by reinforcing the provider’s plan of care. Information exchanged between provider and patient is enhanced with the care manager’s capacity to coach members whose care is complicated by poor health literacy. Care managers also reiterate the need for preventative care and appointment attendance. With the information gathered from the ICM assessment, we send providers a plan of care letter that includes a member’s goals, medications, and barriers to care.
If you have HUSKY Health patients who receive ICM services, please return their care plan to us with acknowledgment and additional comments as desired.
To make a referral to ICM:
There are several ways that providers can refer their members to the ICM program including using the Provider Line at 1.800.440.5071, when prompted, dial extension 2024 to request ICM services.
Providers may also complete and fax an “ICM Referral Form” to 1.866.361.7242. To download the form, visit portal.ct.gov/husky, click “For Providers,” “Provider Forms” under the “Reports & Resources” menu item, then select “ICM Referral Form.”
Reference:
My 9 Months. March of Dimes. http://www.marchofdimes.org

Intensive Care Management – Community Health Workers: Providing Health Education to Support Behavior Modification
Good health starts in our homes and communities. Good health involves addressing more than medical concerns. It involves getting access to healthy food, feeling safe in our homes and schools, and receiving positive social support and interactions from our communities. The Intensive Care Management (ICM) team helps HUSKY Health members address these social determinants of health. . . read more
Social determinants of health can include:
- Availability of resources to meet daily needs (e.g., safe housing and food security)
- Access to healthcare services and health education
- Socioeconomic conditions (e.g., concentrated poverty and the stressful conditions that accompany it)
- Language/Literacy
- Culture
Community Health Workers (CHWs) are integral members of the ICM team. They are non-clinical, community-based, frontline staff who work under the direct supervision of the ICM nurse managers. CHWs work across the continuum of prevention strategies identified below in the Centers for Disease Control and Prevention (CDC) Health Impact Pyramid, primarily focusing on socioeconomic factors, but also supporting healthcare professionals.
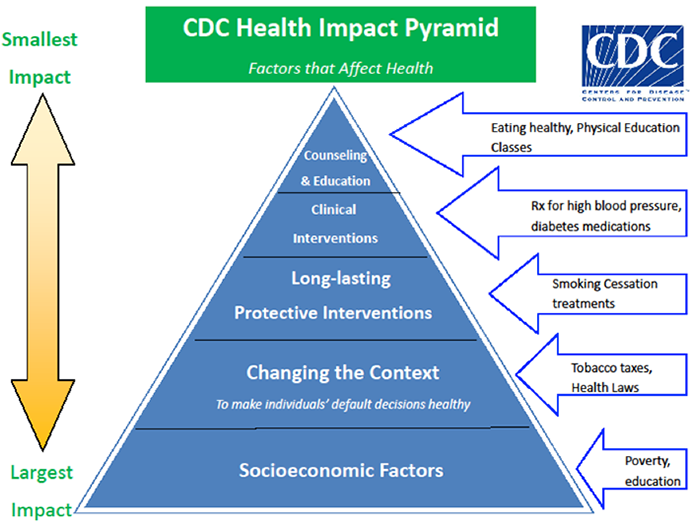
Source: Frieden, T. A Framework for Public Heath Action: The Health Impact Pyramid. Am J Public Health. 2010; April; 100(4): 590–595.
The CHW team has a set of distinct skills including the ability to establish supportive relationships based on shared life experiences and a unique knowledge of the community. CHWs accomplish this by conducting a thorough screening assessment, collaborating with members to establish goals, meeting members “where they are” in the community on face-to-face visits, and providing and reinforcing health education to members so they may become empowered and advocate for their needs.
By addressing the member’s non-clinical needs, the CHW opens the door for the care manager to provide the member with:
- Condition-specific education
- Guidance on the benefits of taking medications as prescribed
- Coaching on self-management skills
- Assistance to facilitate care coordination needs
CHWs are an essential part of the healthcare team. They deliver customized information, viable resources, self-advocacy skills, and improved access to services. All of these help HUSKY Health members to minimize social stressors and redirect members to focus on their improved health outcomes.

Leverage the Provider Collaborative!
Community Health Network of Connecticut, Inc. (CHNCT) offers a comprehensive Provider Collaborative program available to Connecticut Medical Assistance Program (CMAP) providers. As the medical Administrative Services Organization (ASO) for the HUSKY Health program, CHNCT offers a variety of support and services to CMAP providers and HUSKY Health members. . . read more
One of the biggest challenges is ensuring that both providers and members use all of the services that CHNCT offers. The Provider Collaborative is CHNCT’s program to educate providers on the ways that we can help providers as they participate in the CMAP program and manage their HUSKY Health members.
At any time, your practice may request a session with any one of CHNCT’s functional areas:
- Provider Engagement Services – the first line of support for providers who have questions about managing the administrative requirements of the HUSKY Health program
- Member Engagement Services – CHNCT’s representatives are ready and able to help members and providers access benefits and navigate services
- Intensive Care Management – comprehensive care coordination services provided by CHNCT nurse Care Managers to support members with complex and chronic conditions
- Community Support Services – CHNCT offers Community Health Workers to assess member socioeconomic needs and provide education and coaching to access community resources and care coordination services
- Transitional Care – CHNCT’s Transitional Care nurses provide support to members during and after a hospital admission and following an Emergency Department visit
- Prior Authorization – CHNCT is dedicated to providing timely review of medically necessary services requiring prior authorization; our clinical reviewers and non-clinical staff utilize a person-centered approach to the review process
- Community Practice Transformation & Network Management – The State of Connecticut offers a unique Person-Centered Medical Home program which both incentivizes primary care practices for their participation and provides consultative know-how from well-versed medical home experts at no cost to the practice, while also improving quality of care
- Medical Economics & Quality Management – This department is responsible for data reporting, analysis, and clinical evaluation of health outcomes by implementing provider interventions focused on improving the health of the members we serve
For more information click here or go to portal.ct.gov/husky, click “For Providers,” then select “Provider Collaborative” under the “Reports & Resources,” menu item. To leverage the Collaborative for your practice, please call 1.800.440.5071 or email us at provider@chnct.org.

Avoid Payment Interruptions – Keep Your Provider Information Up-to-Date
Have you updated your information lately? All demographic changes for you and your practice, including additions and terminations of physicians, nurse practitioners, and physician assistants, need to be made in a timely fashion to ensure the integrity of the provider directory. These updates assist physicians and clinical staff, call center staff, and members when searching for or referring to a provider to access and coordinate care. . . read more
The accuracy of your provider information may impact the payment of claims and can also affect misdirected payments, the loss of provider eligibility or the recoupment of previously paid claims.
Any changes in address, licensure, provider specialty, certification, business name or ownership, group/clinic affiliation, and Federal Employer Identification Number (FEIN) of all National Provider Identifier (NPI)/medical providers must be communicated to DXC Technology.
The Provider Manual is located on the DSS website and provides more information about managing and updating your provider information. You can access the DSS Provider Manual by clicking here or visiting www.ctdssmap.com, clicking “Information,” then “Publications.”
Please review and update your information by logging into the DSS Provider Portal by clicking here or by going to www.ctdssmap.com and clicking “Secure Site,” on the left-hand navigation menu.
You may also submit any changes, on your letterhead, by mail to:
DXC Technology
P.O. Box 5007
Hartford, CT 06104
PCMH Program Providers Please Note: If you are a provider participating in the DSS PCMH program, you should not update your address through the DSS Provider Portal. Please contact your Regional Network Manager directly or call 203.949.4194 to avoid any missed enhanced payments.
Get to Know Your Provider Engagement Services Representatives
The Community Health Network of Connecticut, Inc. (CHNCT) Provider Engagement Services staff is dedicated to working personally with your practice on site and by phone. Our staff is on the road 4-5 days a week, visiting provider offices to discuss topics such as enrollment/attestation processes, DSS bulletins and policies, HUSKY Health policies and programs, and other important matters. . . read more
Our goal is to establish an open dialogue with you and your practice to promote positive relationships through communication, problem resolution, and education. CHNCT collaborates with our partners at DSS and DXC Technology (formerly Hewlett Packard Enterprises) to address any and all inquiries as quickly as possible and to facilitate resolutions when necessary.
The CHNCT Provider Engagement Services staff supports and attends a number of provider conferences held throughout the state each year. When you see us at an event, please stop by to introduce yourself and we will do the same!
To set up an appointment with us or to speak with your local Provider Engagement Services representative, please call your regional contact listed below:






