Provider Collaborative
The HUSKY Health program is committed to providing support to Connecticut Medical Assistance Program (CMAP) providers.
Additional Resource
CHNCT Provider Collaborative Program
Community Health Network of Connecticut, Inc.® (CHNCT), on behalf of the Department of Social Services (DSS) and the HUSKY Health program, offers a comprehensive program to support Connecticut Medical Assistance Program (CMAP) enrolled providers and their practices. The Provider Collaborative assigns CHNCT subject matter experts to work with providers and their staff to support the practice’s operational, administrative, and clinical functions as they relate to HUSKY Health.
Practices may work with any or all CHNCT departments participating in the Provider Collaborative to receive education and training for services available to providers, their staff, and to HUSKY Health members.
To take advantage of the services the Provider Collaborative offers:
Call or email the designated contact in the desired functional area(s) detailed below to schedule an onsite visit or virtual call. For general questions and provider support, please call Provider Engagement Services at 1.800.440.5071, or contact your regional Provider Engagement representative.
Providers interested in becoming CMAP enrolled and leveraging all of the resources provided by CHNCT, please call 1.800.440.5071.
CHNCT Participating Departments:
- Provider Engagement Services
- Member Engagement Services & Escalation Unit
- Care Management
- Population Health Management
- Quality Management
- DSS Person-Centered Medical Home (PCMH) Program
- Prior Authorization
Provider Engagement Services
CHNCT’s Provider Engagement Services Department is comprised of provider support staff, including regional representatives who are available to work with each provider practice, both virtually and in person. Our goals are to establish an open dialogue with providers and their staff to promote positive relationships through communication and education, and to reduce their administrative burden when possible.
Contact Information
Each regional representative is available to provide exceptional virtual and onsite technical assistance and responsiveness to any concerns identified by provider practices. Providers may request assistance to address any issues with the HUSKY Health program, and our regional representatives will collaborate (as needed) with all program partners, including CHNCT, DSS, and Gainwell Technologies, to bring resolution to the issues as quickly as possible.
We are prepared to discuss any questions providers have, including:
- Changes made to State and Federal Medicaid programs
- DSS bulletins on medical and administrative policies and procedures affecting practices
- Gainwell Technologies’ provider enrollment, attestation, profile updates, and claims resolution
- Reducing missed appointments
- Implementing Telehealth services
Member Engagement Services & Escalation Unit
Member Engagement Services is considered the first line of contact for members and providers regarding any questions about the HUSKY Health program. Member Engagement Services is available Monday through Friday from 8:00 a.m. to 6:00 p.m.
Contact Information
- For Providers: 1.800.440.5071
- For Members: 1.800.859.9889
Member Engagement Services provides assistance with all of the following and more:
- Educating callers on HUSKY Health benefits;
- Assisting with questions on member eligibility;
- Helping members access CMAP enrolled providers, and offering appointment and transportation assistance;
- Referring callers to the Connecticut Dental Health Partnership, Connecticut Behavioral Health Partnership, non-emergency medical transportation, pharmacies, and other program services; and
- Offering community resources for food assistance, utility assistance, shelter, and other non-medical needs.
Member Engagement Services Escalation Unit
The Member Engagement Services Escalation Unit has special expertise with helping HUSKY Health members with the more difficult access to care issues. This includes access to providers in specialty areas such as orthopedics and pain management. The Escalation Unit works directly with providers, members, and their families to support their needs, and assists with scheduling appointments, coordinating transportation to medical appointments, and identifying needed community resources.
Contact the Escalation Unit directly
Providers are encouraged to contact the Escalation Unit directly when members need additional help addressing access to care issues. To initiate services with the Escalation Unit, please do one of the following:
- Download the Escalation Referral form, complete, and fax to 203.265.3197, or email to reachforescalation@chnct.org
- Call us at 1.800.440.5071 and ask for the Escalation Unit
Care Management
The Care Management program, which includes Intensive Care Management and Transitional Care Management, provides comprehensive care coordination services for members with high-risk or complex needs in collaboration with members, their providers, and multidisciplinary teams. Care Management interventions aim to increase member engagement in ongoing care with a primary care provider, decrease potentially avoidable acute care utilization, and reduce health disparities.
Contact Information
For ICM Referrals call 1.800.440.5071 x2024
Refer members to ICM
Providers may refer members to ICM by calling 1.800.440.5071 x2024, or by faxing in a completed ICM Referral Form.
Intensive Care Management: Intensive Care Management focuses on optimizing the health and quality of life of members with complex, co-morbid physical and behavioral health conditions, who are at the highest risk for adverse health outcomes, members with high-risk pregnancies and babies who spent time in the Neonatal Intensive Care Unit after birth, and members with complex care coordination needs, including those obtaining gender-affirming care or organ transplant services. This is accomplished by providing person-centered, culturally competent education, coaching and support; minimizing obstacles to accessing care; and promoting the member’s ability to build trust and engage with the care team. Intensive Care Managers incorporate evidence-based practice guidelines to formulate person-centered care plans, to best support members in achieving their health goals by enhancing their understanding and ability to participate in recommended care.
Transitional Care Management
The goal of this team is to reduce hospital readmissions with a focus on unattributed members with certain risk factors, including chronic and multi-morbid conditions, who have increased readmission rates and risks.
Contact Information
1.800.859.9889 x2011
Transitional Care Management focuses on safe and effective care transitions across settings. The Transitional Care team collaborates with members, caregivers, providers, hospital care teams, and community agencies to ensure provider follow-up and services are in place for members following emergency department (ED) or hospital discharge.
The team’s readmission risk mitigation interventions include:
- Facilitating timely post-discharge follow-up with the provider, either in-person or via telehealth within seven days of discharge. The team works with provider offices to schedule follow-up appointments and helps to arrange non-emergency medical transportation when needed
- Conducting medication reconciliation to assess the member’s ability to take their prescribed medications correctly and consistently, by reviewing claims data, hospital discharge information (if applicable), and member self-reported information
- Evaluating the member’s understanding of discharge instructions through the use of “teach back”
- Utilizing evidence-based tools, such as the Asthma Action Plan and Asthma Control Test™ (ACT™), to educate members about warning signs of exacerbation and promote early treatment
Click here for more information on Transitional Care.
Asthma Control Test is a trademark of QualityMetric Incorporated. The Childhood Asthma Control Test was developed by GSK.
Population Health Management
The Population Health Management Department is responsible for data reporting, data analysis, clinical evaluation of health outcomes, and the supporting analysis for implementation of provider interventions focused on improving the health of the members we serve.
Contact Information
The Population Health team conducts and analyzes various reporting measures, which include both the HEDIS® and CMS core set of Adult and Child Health Care Quality Measures. The team is also responsible for large project reporting and analysis that is requested by DSS. These projects range from designing new reimbursement methodologies (bundled payments), to risk score based analysis to assign populations to a specific risk population stratification, and anything else as requested by DSS.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA)
Quality Management
The Quality Management (QM) Department manages the implementation and evaluation of CHNCT’s comprehensive QM program. The program addresses service quality and clinical quality, member and provider interventions, and performance improvement strategies as they pertain to the specific healthcare needs of the adult and child Medicaid and Children’s Health Insurance Program (CHIP) populations enrolled in the HUSKY Health program.
Contact Information
The QM program is annually developed in collaboration with DSS to ensure that all HUSKY Health members receive medically necessary and cost-effective treatment to maximize their health outcomes. Opportunities to address health equity and social drivers of health (SDOH), which are fundamental to improving health outcomes program-wide, are embedded into all aspects of the annual QM Work Plan. All quality activities are conducted in accordance with Utilization Review Accreditation Commission (URAC®) standards.
In addition to the QM program activities and the accreditation responsibilities, the QM team is responsible for the following:
- Evaluating clinical health outcomes and trends related to the various Medicaid quality metrics to determine member and/or provider interventions that can enhance the HUSKY Health program experience
- Identifying opportunities and addressing barriers related to SDOH to close gaps in care and promote health equity among members
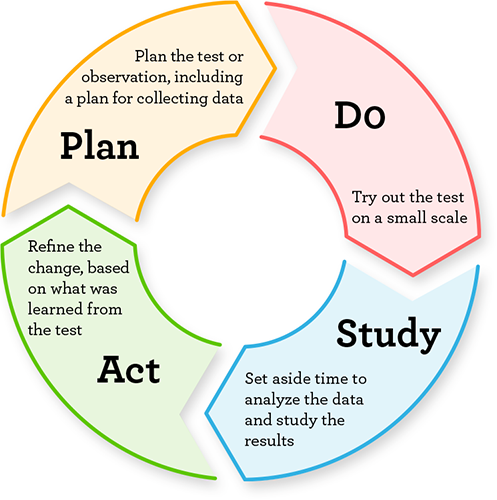
- Conducting root cause analyses, creating plans for improvement, implementing interventions, assessing performance improvement, and providing clinical observations based on the outcome of interventions
- Monitoring and evaluating active Quality Improvement Projects (QIPs) through outcome reporting, and incorporating effective interventions into existing workflows
- Working with provider practices on quality improvement opportunities to improve member health outcomes, and supporting the program requirements outlined in the NCQA Patient-Centered Medical Home (PCMH) recognition and The Joint Commission (TJC) PCMH certification
- Providing guidance to practices engaged in the DSS Person-Centered Medical Home (PCMH) program in obtaining and/or maintaining recognition/certification
- Supporting PCMH+ practices with reporting and member resources while collaborating with DSS on program details
- Investigating and conducting quality of care reviews and adverse event reporting to DSS and the Department of Public Health (DPH) as necessary to support and address patient safety efforts among HUSKY Health members
- Collaborating with other internal departments to meet program goals and objectives outlined within the QM program to analyze and report on health measures and Medicaid quality metrics
DSS Person-Centered Medical Home (PCMH) Program
The DSS Person-Centered Medical Home program is designed to improve patient quality of care. Support for the providers to accomplish this goal comes from financial incentives, technical assistance, and instruction to achieve PCMH recognition and education, with hands-on guidance to implement and support quality improvement within primary care practices. Medical homes can improve the quality of care, especially for patients with multiple chronic conditions due to National Committee for Quality Assurance (NCQA) requirements of care coordination activities and quality improvement efforts.
Contact Information
Call 203.949.4194 or email at pathwaytopcmh@chnct.org
The program encompasses the following framework:
- Providing members with the information, education, and support needed to make fully informed decisions about their care options, and to actively participate in their self-care and planning
- Supporting the member, and any representative(s) they have chosen, in working together with their non-medical, medical, and behavioral health providers, and care manager(s) to obtain necessary supports and services
- Reflecting care coordination under the direction of, and in partnership with, the member and their representative(s); that is consistent with their personal preferences, choices, and strengths, and that is implemented in the most integrated setting
- Guiding practices in the use of reports and gap analysis tools to implement processes and procedures that improve the care of patients and make practices more efficient
The Clinical Practice Transformation Specialists (CPTS) and other PCMH program staff are a vital component of the CHNCT QM program. They are responsible for assisting primary care practices with their applications and reporting requirements to the DSS Person-Centered Medical Home (PCMH) and/or DSS Glide Path programs to become PCMH recognized practices. The CPTS team is trained specifically on Nationally Accredited PCMH Standards and maintain NCQA PCMH Content Expert Certification™. Their skill set also includes quality improvement and practice transformation activities to support primary care providers in improving patient health outcomes at the practice level.
Education and support to practices regarding NCQA PCMH recognition and TJC PCMH certification process are provided to those practices enrolled in the DSS PCMH and Glide Path programs. CMAP primary care practices are provided with training and assistance on the various analytical tools and reports available for Medicaid population health management by CHNCT. Providers use these tools and reports to identify their members with gaps in care, as well as those who may benefit from care coordination. Practice outreach to members may help to improve health outcomes by encouraging needed services from the established relationship that is cultivated through the PCMH care model. In addition, CPTS staff support all CMAP practices with the quality improvement processes and interventions. The PCMH program staff contact primary care practices that qualify for the DSS PCMH program to introduce the PCMH model of care, including specific information on NCQA PCMH recognition and the DSS PCMH program. For more information on becoming a PCMH, please click here.
This portion of the HUSKY Health website is managed by Community Health Network of Connecticut, Inc.®, the State of Connecticut’s Medical Administrative Services Organization (ASO) for the HUSKY Health program. For the general HUSKY Health website gateway, please visit portal.ct.gov/husky. HUSKY Health includes Medicaid and the Children’s Health Insurance Program, and is administered by the Connecticut Department of Social Services (DSS).