Quality Improvement
Quality Improvement (QI) is essential for a Patient-Centered Medical Home (PCMH) practice, both in obtaining recognition and more importantly, in maintaining it. QI can help improve patient care and may help you qualify for the PCMH Performance-Based Payment program for additional financial incentives.
List of topics:
Introduction to Quality Improvement
Engaging in QI activities is critical to achieving the quadruple aim of improving the health of the population, enhancing patient experiences and outcomes, reducing the per capita cost of care, and improving provider experience. Many providers, insurers, delivery systems, and QI organizations are focused on improving the performance and safety of primary care.
For many practices, QI is likely to be a new activity. As with the implementation of many new ideas and processes, practices will need new skills to meet their improvement goals. External supports can help practices learn these new skills and better implement QI. These supports include data feedback on key indicators and practice facilitation (or coaching) to help build the capacity for QI.
Learn about QI supportsHelp and Support
Community Practice Transformation Program Team
Community Health Network of Connecticut, Inc.® (CHNCT) has a team of trained staff to help and support you!
They will assist you with your practice needs for PCMH and QI. This service is at no cost to your practice.
To reach our team, call 203.949.4194 or email pcmhglideapplication@chnct.org.
Continuous Quality Improvement for Primary Care Practices
Continuous Quality Improvement (CQI) begins with the culture of improvement for the patient, the practice, and the population in general. The culture begins with a QI team led by a clinical practice champion.
Your assigned Clinical Practice Transformation Specialist (CPTS) can support you as a practice facilitator. They can assist you with completing an assessment to help you identify current needs and develop your practice’s capacity for improvement to address these needs. A facilitator can tailor QI efforts to your practice and help implement them.
Practice Facilitator SupportCQI is a philosophy that encourages all healthcare team members to continuously ask:
- Can we be more efficient?
- Can we be more effective?
- Can we be faster?
PCMH and Quality Improvement
PCMH involves numerous changes – to processes, workflows, scheduling systems, and the care team structure. PCMH supports QI in primary care by acknowledging the core concepts set forth by the National Committee for Quality Assurance (NCQA). QI is integrated into each of the six NCQA PCMH concepts. The concepts contain specific criteria that outline the features of the practice’s transformation to a PCMH.
- Team-Based Care and Practice Organization (TC)
- Knowing and Managing Your Patients (KM)
- Patient-Centered Access and Continuity (AC)
- Care Management and Support (CM)
- Care Coordination and Care Transitions (CC)
- Performance Measurement and Quality Improvement (QI)
For more information, e-mail pcmhglideapplication@chnct.org.
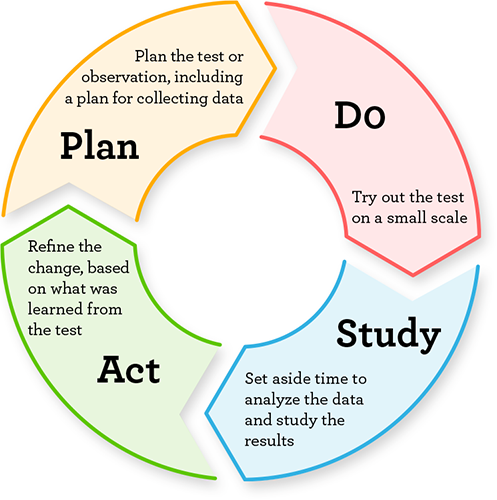
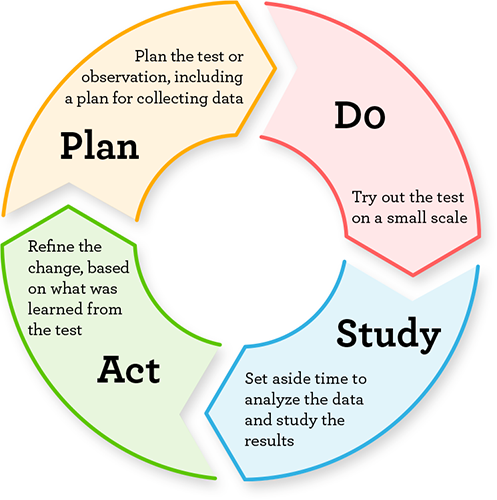
The Plan-Do-Study-Act Cycle
The Plan-Do-Study-Act (PDSA) cycle is a tool for CQI. The goal of the PDSA cycle is to test a change – by planning it, trying it, observing the results, and acting on what is learned.
Using your Electronic Health Record for Quality Improvement
Many Electronic Health Records (EHRs) can help you with QI in ways that save your practice time and money. Although each EHR system is unique, below are links that may assist with QI. EHRs can improve healthcare quality. EHRs can also make healthcare more convenient for providers and patients.
Improve Care Using EHRsElectronic Health Records allow your practice to:
Deliver reliable and efficient care
- Standardized workflow
- Clinical practice expectations are clear
Ensure that everyone gets the care they need
- Care Management
- Detailed “patient panel” reports
Give the right care at the right time
- Point of care reminders/alerts
- Evidence-based treatment options for measures/order sets
Provide timely and credible performance feedback
- Primary caregiver (responsible party) clearly identified
- Reports based on current clinical data
- Flexible query function for getting more specific data within a measure
- Data available for benchmarking
NCQA PCMH Recognition and the Quality Improvement Worksheets
The quality improvement process has a specific set of steps.
Quality Improvement Worksheet
If your practice is working towards initial NCQA PCMH recognition, you can use the Quality Improvement Worksheet to demonstrate the continuous quality improvement process. The worksheet is found in the current NCQA PCMH standards and guidelines which you can order from the NCQA store.
NCQA PCMH Standards and GuidelinesHere are the steps to follow as your practice goes through the process of achieving or sustaining NCQA PCMH recognition:
- Identify measures for QI
- Establish a performance goal
- Identify a baseline performance assessment
- Determine actions to work toward performance goals
- Re-measure performance based on actions taken
- Assess actions taken and describe improvement
This portion of the HUSKY Health website is managed by Community Health Network of Connecticut, Inc.®, the State of Connecticut’s Medical Administrative Services Organization (ASO) for the HUSKY Health program. For the general HUSKY Health website gateway, please visit portal.ct.gov/husky. HUSKY Health includes Medicaid and the Children’s Health Insurance Program, and is administered by the Connecticut Department of Social Services (DSS).